We began the day by making a variety of stains. The first stain we made was a Capsule stain to see if our unknown bacteria had any capsules. We used Nigrosin to stain and added the bacteria, using the aseptic technique, from the working stock to the stain drop. The slide was held at a 45 degree angle to spread the dye and bacteria by dragging another slide across it in one, smooth movement. After drying, safranin was added to cover the slide for 60 seconds. The slide was rinsed with water and blotted dry. The nigrosin stains the background of the cell and the saphrinin
stains the cell wall so that the capsules surrounding them can be clearly seen. Because there was no white and both the bacteria cell wall and background were dyed, there was no capsule. By using this stain method, health science majors can determine the bacteria and properly treat the bacteria.
 |
| Bacteria with no capsule |
The next stain was did was endospore stain to see if our bacteria was producing endospores. We drew a circle of the slide with a china marker to know where to place the bacteria. We added a droplet of water and bacteria from the working stock. Once it was air-dried, the slide was placed over boiling water and covered with bibulous paper. The slide was saturated with malachite green dye for 5 minutes. After the malachite green began to steam,
adding additional stain to the slide to prevent it from drying. After 5 minutes, the paper was removed from the slide and placed in the biohazard bag. The slide was left to cool. It was rinsed with water then covered with safrinin fro 60 seconds and rinsed with water again to removed excess safranin. The slide was blotted with bibulous paper. After examining the slide under the microscope, there was no endospores.
 |
| Saturating with malachite green |
 |
| Rinsing the slide |
 |
| Bacteria under the microscope |
 |
| No Endospores! | | | |
|
|
Our next stain was the acid-fast stain. After preparing a slide with our bacteria using the aseptic technique, the slide was placed over a beaker with boiling water. Bibulous paper was placed over the slide and saturated with Ziehl-Neelson carbolfuchsin. The stain was covered for 4 minutes. While the stain was evaporating, more stain was added to prevent it from drying. After 4 minutes, the slide was removed from the heat to cool and the paper was placed in the biohazard bag. To remove excess stain, the slide was rinsed with water. The slide was held at a 45 degree angle and decolorized with acid alcohol. The slide was rinsed with water and then covered with methylene blue for 2 minutes. The slide was rinsed with water and blotted dry with bibulous paper.
 |
| Saturating the slide with Ziehl-Neelson carbolfuchsin |
 |
| Bacteria under the microscope | | | | | | | | |
| |
|
|
|
|
|
|
|
|
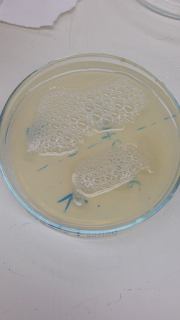
The next part of the day consisted of doing a multitude of test to determine our unknown bacteria.
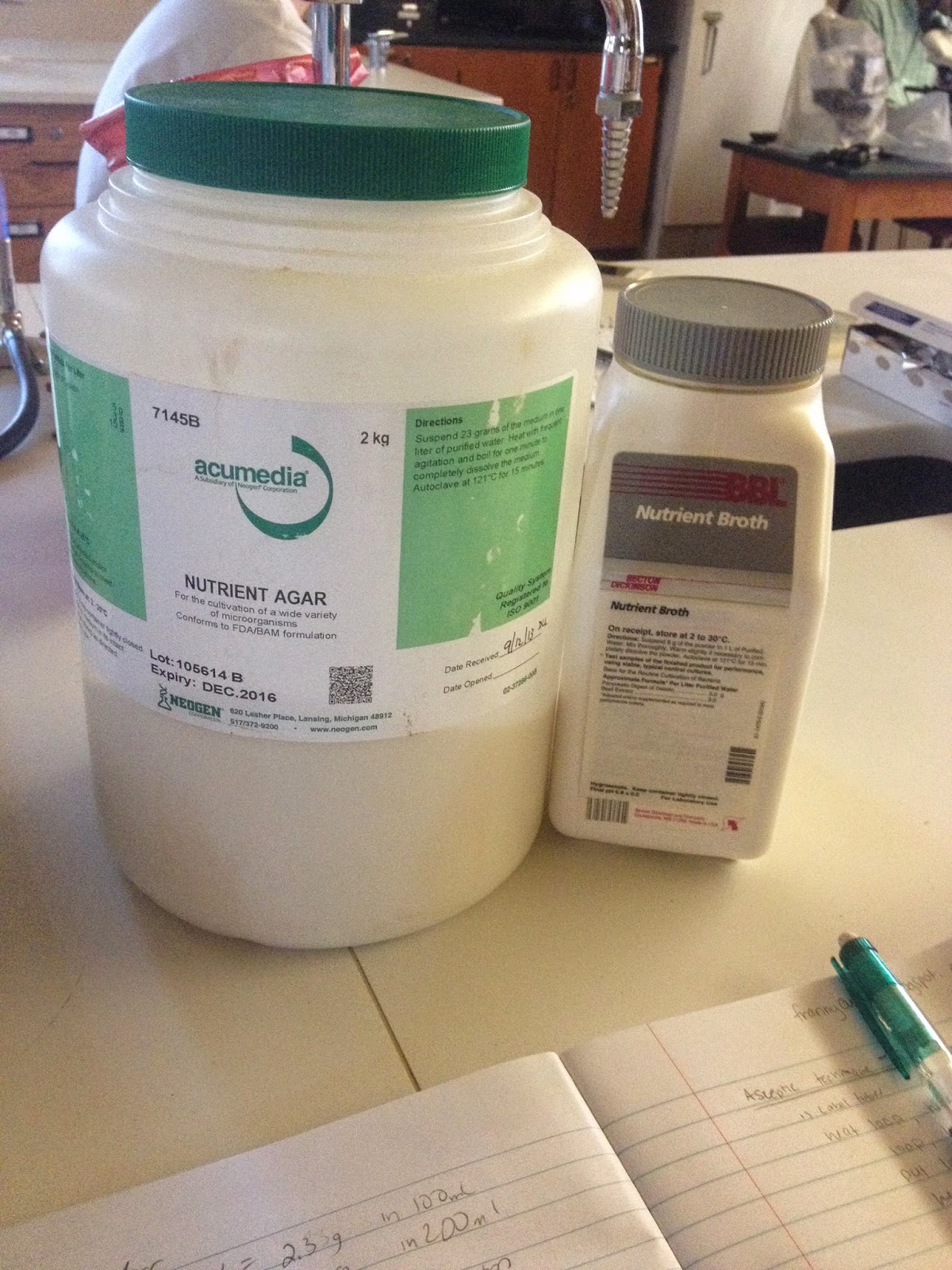
Our first test was the starch hydrolysis test. This test would determine if our bacteria contain amylase, which digest starch. Using a starch agar plate, we inoculated it by streaking a squiggle like on the surface using the working stock culture. We incubated the plate at 37
°C overnight.
We preformed the casein hydrolysis test to see if our unknown bacteria contained caseianse, a protease that digests casein (how clever!). We inoculated a skim milk agar plate by streaking a squiggle line on the surface of the agar with our working stock culture. The plate was incubated at 37
°C overnight.
Next, we did the urea hydrolysis test, the lipid test, to see if our bacteria contained urease. We used urea-containing broth. Using the aseptic technique, we inoculated the urea with our working stock culture. The tube was incubated at 37
°C overnight.
Next was the gelatin hydrolysis test. Using a nutrient gelatin test tube culture, we stabbed the nutrient gelatin with our bacteria, inoculating it. We incubated the tube was incubated at 37
°C overnight
.
Our next experiments involved a variety of sugars. We inoculated three sugar test tubes to determine our unknown bacteria’s ability to
ferment certain carbohydrates. The sugars used were lactose, glucose, sucrose, and mannitol. Using the aseptic technique, the bacteria from our working stock cultures were inoculated into each tube, respectively. We did a mixed acid test of methyl-red and Voges-Proskaus. Using the
aspetic technique, we used the working stock culture to inoculate the
liquid culture. We used the same technique for the indole (tryptophan)
and nitrate cultures. The next culture was the citrate slant. Using the aspetic technique, a needle of bacteria form our working stock culture was inoculated into the tube.
 |
| Our sugar tubes |
Next, we tested our bacteria using the “Triple Sugar Iron
Agar” or “TSIA” using the same technique as above.
Another test we performed was the Litmus milk test. The test allowed us to find out whether our bacterium utilizes proteins, lactose
and litmus.
The next part of the day consisted of determining if our unknown was
facultature, meaning both aerobic and anaerobic. We known that our
culture is not obigate anaerobic because our unknown bacteria has grown
in oxygen (aerobic). In order to test if our unknown is facultature, we
did a multitude of tests.
To test for motility, we used the aseptic technique by dipping our inoculating needle into the working stock culture. We stabbed the needle into the middle of the motility medium. The tube was incubated at 37°C overnight.
For the catalase test, after the aspetic technique, we drew a squiggle like of a nutrient agar culture plate. The plate was incubated at 37
°C overnight.
Finally, we wanted to determine if our unknown was
facultature, meaning both aerobic and anaerobic. We known that our
culture is not obigate anaerobic because our unknown bacteria has grown
in oxygen (aerobic). In order to test if our unknown is facultature, we
did gaspac and thyoglycolate tests. For the gaspac test, after the aspetic technique, we drew a squiggle like of a nutrient agar culture plate. For the thyoglycolate test, after using the aspetic technique, we obtained bacteria from the working stock culture and inoculated the thyoglycolate tube. The tube was incubated at 37
°C overnight.
 |
| Placing our cultures under anaerobic conditions |
The pictures of these tests are seen in the Day 4 post!